 |
BMe Research Grant |

|
Géza Pattantyús-Ábrahám Doctoral School of Mechanical Engineering
Department of Machine and Product Design
Supervisor: Dr. Károly Váradi
Finite element modeling of mandible reconstruction
Introducing the research area
In case of oral cavity tumors, early detection can be a life-saver. Approximately 3000 people are diagnosed with oral cavity tumor each year in Hungary, while 1700 can be associated with early death. The pathological deviations of oral cavity are among the tumors easiest to detected,and in case of late discovery, due to the radical interactions, the chance of recovery decreases. Oral cavity tumors occur more frequently above ago of 50. Over the past years, both the occurrence of the illness and the death rate have risen! Therefore, early detection is very important.
My field of research is the most frequently occurring branch of the tumor, which is the jaw, jawbone (mandible) and their resection, reposition and fixation using implants technology.

Fig. 1. Mandible tumor
These surgical techniques and their stability insurance information were collected using cadaver, bone-ligament laboratory measurements in earlier times. These investigations can be rather difficult, not to mention legal/ethical problems concerning dead people. Nowadays, the use of finite element analysis is more and more popular. Correctly built models with real material properties can be very effective and helpful in clinical fixation techniques and tests used in practice. This technology can also accelerate the healing and recovery time of patients and their life conditions after the surgery.
Brief introduction of the research place
Mechanical Engineering Department is among the largest departments at the Budapest Technology and Economics University. Additionally to the regular research works, the Department is involved in many external industrial problems, therefore, there are a wide variety of engineering activities associated. The Department is involved in biomechanical research for many years.
History and context of the research
Unlike in reconstructional dentinal implants, there are few investigations and documentations in oral surgery regarding mechanical reconstruction of the jaw tumor resection. The investigations and test focus precisely on the breakage of the implants and the tear effect of the fixing screws for the plates. Plate geometries, built on more complicated geometry compared to the those of bone, are mainly handled with in a simplified form throughout the literature dealing with this topic. This is also true in case of the compound screw geometries. However, the palette of bones models used in finite element analyses is very wide, depending on the design of the bone structure modeling during the test. In the literature, these bone substances are defined with homogen linear elastic behavior. The main substance types are the cortical (hard) and spongiosa (spong) areas. There are several methods in the design of geometry, ranging from models constructed from geometric primitives, to medical imaging systems (MRI, Computer Tomography), and to the hybrids of multiple methods.
The goal of the research and open questions
I prepare my thesis in collaboration with international and local universities (e.g. Semmelweis University (Budapest), Military Hospital – State Health Centre (Budapest), University Hospitals of Leicester, University of Leicester (UK), Regea Institute for Regenerative Medicine, University of Tampere and University of Oulu (Finland), Mid Sweden University, Östersund (Sweden)).
My goal is to preliminary examine reconstruction solutions on straight bone (human radius) using partial, arbitrary geometrical resection.
My research focuses on finite element analysis of the most frequently used general reconstruction technique with plates and screwing systems in case of jaw reconstruction.
I include the main resection domains used in the clinical practice. During modeling, my aim is to achieve more accurate geometry that can be found in literature. The goal is to create a model the closest to reality using CT data and Hounsfield unit that provide realistic results. Validation is done by human mandible bone samples tested with press machine. When designing the model, an important aspect was to ensure possibility of modification of screw geometry, whenever required, furthermore, to decrease the computing capacity requested for the modification of implant geometries in the sub models. After the results evaluation, I would like to make a recommendation for the optimization of existing implants and for the creation of a new implant supporting ossification, and possibly produce a prototype.
Methods
To reinforce jaw, in many cases human bone is used. The source of such bone can be for example the human radius. The stability of radius decreases after removing the bone fragment (partial resection), which needs to be mechanically reconstructed, similarly to the full resection. During my preliminary examinations, I created models of the partial reconstruction of straight bone so that the 4 different fixation techniques can be compared. Inside the 4 global models, I allocated sub models with variable resection geometries. The examination was focused on the 4 point bending and torsion cases.



Fig. 2. Human radius reconstruction
The
design of the geometrical model is based on the point clouds generated in computer tomography, and which were imported to CAD environment after
fine-tuning, segmenting and correction. In this environment, I created
the base model for the finite element analysis.
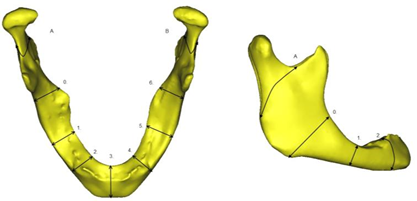
Fig. 3. Main resection areas
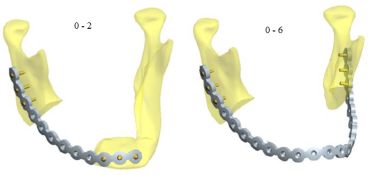
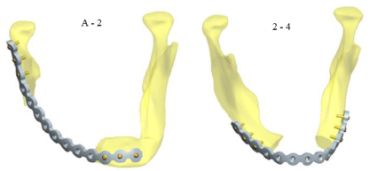
Fig. 4. Mandible reconstructions
In the simulation, investigations can be divided into two main categories: global model and (so-called) sub model related investigations. During the global model investigations, screw thread geometries are simplified to speed up computing; however, these geometries are implemented in the sub model situation. I used bone samples from human mandible in the press machine to validate the heterogeneous material structure used as a base of the simulations. Material properties were defined using regressive cross-compliance functions based on the results from computer tomography points carrying the Hounsfield units. After the definition, they were allocated to the finite element mesh, enabling different properties assigned to each element.
In this way a very realistic picture can be deducted about the different mechanical behavior in the area of the fixing screws. Based on the related literature, the Young-module of the bone is 0-23000 MPa, which is divided in this range with constant 0.3 Poisson coefficient in the this case. Linearly elastic isotropic material properties were used during the investigation.
Boundary conditions and loads represent chewing forces for examinations. Chewing is a very complicated movement that comes from complex muscle operation. The main elements were applied on the model based on anatomical method.
Fig. 5. Main chewing muscles
Results
During my research, I used jaws pieces from dead bodies, and placed validation elements with known density required for the CT scans. In the evaluation I proved that there is no significant difference in the density values used for the creation of the heterogeneous material structure when using Cone Beam Computer Tomography (50-100 times less radiation) and Medical Computer Tomography (traditional, higher radiation).
I made CT scan on human jaw bone samples (cylinders), then tested them on press machine to get further information required for the optimization of models applied at my earlier biomechanical examinations, and for the development and validation of finite element bone models. I compared the examination to computer supported simulation, and I concluded a more punctual heterogeneous value (which has a very wide range in the current literature) of the elastic modulus of the load carrying hard allocation of the bottom jawbone.

Fig. 6. Compression test of bone samples
I created a complex finite element model of major jawbone resections applied in clinical practice, where the area of screws for direct plate technique using sub model situation can be investigated, supporting this way the screw implants and correct geometrical design regarding the load in the bone. The parametric model also contains the complete screw geometry for mono and bi-cortical solution in Lock and Non-Lock systems. Based on the CT results, I created a unique inhomogeneous material property with bone density spectrum. 4 main resection cases were examined with mentioned techniques in case of lower jaw.
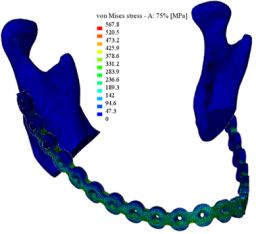
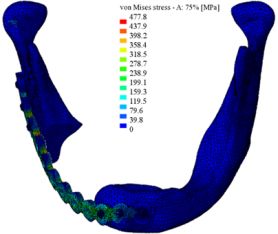
Fig. 7. Von Mises stresses
The introduced methods during the straight bone investigation were developed for human radius bone and detailed for 4 different plating techniques.
From the finished elements tests performed on the mentioned models I gained a good understanding of the stresses generated in jawbone and implants in case of main resection types. These results can be very helpful in the optimal implants design. Proposal can be made about the position of the implants regarding the resection types.
Using the results from the examination of the human straight radius, I identified the fixation technique of the 4 analyzed cases that poses the minimum load. Furthermore, I identified resection type accompanied with the smallest stress in the bone. This partial resection geometrical analysis can be implemented into the jawbone as well.
My existing results provide valuable information for the creation or modification of implant geometries that allow for a faster regeneration of the bone in the future.
Expected impact and further research
The created frame system is capable of investigating graft implants and also existing implants optimization. Also, provides the base for the investigation of new screw geometries depending on the fixation systems. Resection cases used in clinical practice can be analyzed. Furthermore, considering and using the results can help prevent the overload or fracture of bone and avoid the tear out of implants. Also, a more stable fixation can lead to faster recovery. Based on the results, I try to design a bone growth stimuli scaffold structure, where the bone can interact with the implant and grow in or around it, deepening the stability of the structure.
Publications, reference, link collection
Related own publications:
[1] Bujtar Peter, Christopher Avery, Janos Simonovics, George K Sandor, Jingzhe Pan, Refinements in osteotomy design to improve structural integrity: a finite element analysis study. The British Journal of Oral & Maxillofacial Surgery 10/2012; DOI:10.1016/j.bjoms.2012.09.015. IF= 2.717
[2] C. M. E. Avery, P. Bujtár, J. Simonovics, T. Dézsi, K. Váradi, G. K. B. Sándor, and J. Pan, A finite element analysis of bone plates available for prophylactic internal fixation of the radial osteocutaneous donor site using the sheep tibia model. Med. Eng. Phys., 2013 Apr 23. pii: S1350-4533(13)00076-3. doi: 10.1016/j.medengphy.2013.03.014. IF= 1.623
[3] Bodzay, T., G. Sztrinkai, T. Gál, J. Simonovics, and K. Váradi (2013). How Bilateral Iliolumbar Fusion Increases the Stability of Horizontal Osteosynthesis in Unstable Pelvic Ring Injuries? Archives of Orthopaedic and Trauma Surgery. ISSN: 0936-8051. DOI: 10.1007/s00402-013-1762-1. IF= 1,37
[4] Simonovics János, Dr. Váradi Károly, Dr. Bujtár Péter, Biomechanikai csontmodell építésének lehetőségei (in Hungarian). GÉP, Vol. LXII. (2011/11), No. II. pp. 24-27 (ISSN 0016-8572)
[5] Simonovics János, Dr. Váradi Károly, Dr. Bodzay Tamás, Study and examination of the implements used for securing pelvis bone. Biomechanica Hungarica, 2010. III/1; pp. 215-223 (ISSN 2060-4475)
[6] Simonovics János, Dr. Váradi Károly, Dr. Bodzay Tamás, Medencetörés rögzítési technikák vizsgálata (in Hungarian). GÉP, LXI. Vol. (2010/9-10), I. pp. 90-93. (ISSN 0016-8572)
[7] J Simonovics, K Váradi, Finite element analysis of the lower jaw implant in different resection scenarios. Pollack Periodica, Vol.8.No.2. (2013) (in press) ISSN: 1788-1994
[8] J Simonovics, P Bujtár, K Váradi, Effect of preloading on lower jaw implant. Biomechanica Hungarica, 2013. VI/1; (ISSN 2060-4475)
[9] Simonovics János, Dr. Váradi Károly, Dr. Bodzay Tamás, Massa lateralis medencetörés implantátumainak vizsgálata (in Hungarian). OGÉT 2010 XVIII. Nemzetközi Gépészeti Találkozó, Nagybánya, Romania, April 22-25, 2010, pp. 372-375. ISSN: 2068-1267.
[10] J Simonovics, P Bujtár, GK Sándor, K Váradi, Study of a customized lower jaw implant. OGÉT 2012 XX. Nemzetközi Gépészeti Találkozó, Romania, April 21, 2012, pp. 402-405. ISSN: 2068-1267.
[11] J Simonovics, P Bujtár, CME Avery, GK Sándor, J Pan, K Váradi: Study and examination of the implements used for prophylactic internal fixation. GÉPÉSZET 2012, Budapest,May 24-25, 2012, pp. 482-487. ISBN: 978-963-313-055-1
[12] Simonovics János, Dr. Bujtár Péter, Dr. Váradi Károly, Effect of bitting in case of lower jaw implant loading. OGÉT 2013 XXI. Nemzetközi Gépészeti Találkozó, April 25-28, 2013, Arad, Romania. pp. 342-345. ISSN: 2068-1267.
[13] P Bujtár, CME Avery, J Simonovics, GK Sándor, O Lukáts, A Szűcs, G Zombori, A two phase human follow-up study with ceramic porous implants made of hydroxyapatite (HA) and aluminium-oxide. -A method for CBCT/DVT standardization and histology assessment. BAHNO – British Association of Head and Neck Oncology 2012 – 27th April, London, UK.
[14] Bujtár P, Avery CME, Simonovics J, Sándor GK, Pan J, Váradi K, The relative strengths of differing types of osteotomy design. BAHNO – British Association of Head and Neck Oncology 2012 – 27th April, London, UK.
[15] Avery CME, Bujtár P, Simonovics J, Sándor GK, Pan J, Váradi K, A finite element analysis of the plates used for prophylactic internal fixation of the radial osteocutaneous donor site. BAHNO – British Association of Head and Neck Oncology 2012 – 27th April, London, UK.
[16] Christopher Avery, Péter Bujtár, János Simonovics, Tamás Dézsi, Andrew Peden, Jingzhe Pan, Károly Váradi, Attila Bojtos, Claire Robinson, Finite Element Analysis of Bone Plates Suitable for Prophylactic Internal Fixation of the Radial Osteocutaneous Donor Site using a Sheep Tibia Model. 2011 Simpleware Users Meeting, Bristol, Anglia, The Watershed Media Centre, 11/09/2011.
[17] Bujtár Péter, Simonovics János, Sándor K.B., Jan Wolff, Christopher Avery, Szűcs Attila, Barabás József, Hosszú csöves csontokon (mandibula) végzett oszteoszintézisek biomechanikai vizsgálata ((in Hungarian). 8. Nemzetközi Danubius Kongresszus és a Magyar Arc-, Állcsont- és Szájsebészeti Társaság 15. Nemzetközi Kongresszusa, Debrecen - Kölcsey Konferencia Központ, August 25-27, 2011, p. 53
[18] Bujtar P., Sandor GK., Avery C., Simonovics J, Lukats O., A standardized method with CBCT/DVT for porous implant follow-up. A two phase human study with hydroxyapatit (HA) and aluminium-oxide ceramic porous implants. BAOMS - British Association of Oral and Maxillofacial Surgery, 20-22 June 2012.
[19] Bujtár P, Avery CME, Simonovics J, Sándor GK, Pan J, Váradi K., An assessment of the stability of differing types of fixation following segmental resection of the mandible. BAOMS - British Association of Oral and Maxillofacial Surgery, 20-22 June 2012.
[20] J Simonovics, K Váradi, Finite element analysis of the lower jaw implant in different resection scenarios. 8th International PhD & DLA Symposium, Pécs, Hungary, 29th-30th October, 2012
[21] P Bujtar, C Avery, J Simonovics, J Pan, G K Sandor, K Váradi, Biomechanical evaluation of mandible segmental reconstructions using different methods of fixation. 2013.OP111. Oral Oncology 49: S47–S48. ISSN: 13688375. DOI: 10.1016/j.oraloncology.2013.03.119. 4th World Congress of the IAOO (International Academy of Oral Oncology), 15-18 May, 2013. Rhodes Island, Greece
[22] P Bujtar, C Avery, J Simonovics, J Pan, A failure-proof surgical technique for marginal resections and angulated osteotomies? 2013.OP084. Oral Oncology 49: S38. ISSN: 13688375. DOI:10.1016/j.oraloncology.2013.03.092. 4th World Congress of the IAOO (International Academy of Oral Oncology), 15-18 May, 2013. Rhodes Island, Greece
[23] J Simonovics, P Bujtár, Examination of mandible resections from biomechanical point of view. II. Interdisciplinary Doctoral Conference 2013, 15-17. May, 2013. Pécs, Hungary
[24] J Simonovics, P Bujtár, K Váradi - Examinations of lower jaw reconstructions. TAVASZI SZÉL Konferencia (Doktoranduszok Országos Szövetsége), May 31 - June 2, 2013, Sopron, Hungary
Reference list:
[1] Avery, C.M.E., et al., Biomechanical study of prophylactic internal fixation of the radial osteocutaneous donor site using the sheep tibia model. British Journal of Oral and Maxillofacial Surgery, 2007. 45(6): pp. 441-446.
[2] Avery, C., A Review of the Radial Free Flap: Still Evolving or Facing Extinction? Part Two. Osteocutaneous Radial Flap. Br J Oral Maxillofac Surg, 2010. 48: pp. 253-260.
[3] Bujtar, P., et al., Finite element analysis of the human mandible at 3 different stages of life. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2010. 110(3): pp. 301-9.
[4] Ramos, A., et al., The influence of condylar geometry and positions of bone fixation screws on a TMJ implant. Computer Methods in Biomechanics and Biomedical Engineering, 2010. 13: pp. 115-116.
[5] Keller, T.S., Predicting the compressive mechanical behavior of bone. Journal of biomechanics, 1994. 27(9): pp. 1159-1168.
[6] Rho, J.Y., M.C. Hobatho, and R.B. Ashman, Relations of mechanical properties to density and CT numbers in human bone. Medical engineering & physics, 1995. 17(5): pp. 347-355.
[7] Lienau, J., et al., Initial vascularization and tissue differentiation are influenced by fixation stability. Journal of Orthopaedic Research, 2005. 23(3): pp. 639-645.
[8] Shirazi Adl, A., M. Dammak, and G. Paiement, Experimental determination of friction characteristics at the trabecular bone/porous coated metal interface in cementless implants. Journal of biomedical materials research, 1993. 27(2): pp. 167-175.
